Telehealth scales up during the pandemic to offer patient care in the safety of the home
Hailed for its ability to erase distance between health care providers in cities and patients in rural areas, telehealth has ironically enabled medical care to continue in a time when we all must keep our distance.
13 september 2020--Across the country, telehealth use has spiked as providers offer virtual patient visits to ensure medical needs are met while minimizing COVID-19 exposure. Regulatory agencies have loosened some restrictions on telehealth during this crisis, and more and more payers have begun to reimburse for it as they would for any other medical service.
The Medical University of South Carolina, one of only two Telehealth Centers of Excellence nationwide, quickly mounted a four-pronged response to the COVID-19 pandemic that ensured both continuity of care for patients with suspected or confirmed COVID-19 and continued ambulatory, also referred to as outpatient, care for all other patients. The team of telehealth and bioinformatics experts who led the effort documented their approach and its success in a recent article in the Journal of the American Medical Informatics Association.
Early on, MUSC Health and telehealth leaders saw the need for a coordinated response to the pandemic.
"The same realization was coming to the forefront of the minds of the leadership, myself included, in telehealth that this was going to be a big problem," said Dee Ford, M.D., director of the MUSC Telehealth Center of Excellence and lead author on the article. "We needed in our own way to create some kind of response to what we believed to be a pretty significant public health problem. Planning started before we even had a case in the state."
Very quickly, MUSC Health was able to stand up virtual screening of patients with suspected COVID-19 and mobile testing sites across the state, a remote home-monitoring program for patients with less severe COVID-19 and a telesitter program for hospitalized patients that enabled providers to monitor and communicate with patients via an audiovisual monitor, minimizing health care exposure and preserving personal protective equipment.
It was able to do so in part because it had long been building its telehealth and bioinformatics capacity. With generous funding from the state, the MUSC Health Center for Telehealth, in coordination with the South Carolina Telehealth Alliance, has been expanding its telehealth services throughout even the remotest regions of the state.
"The state of South Carolina made an investment in MUSC years ago to develop telehealth programs, which then led to a high state of expertise and readiness to pivot when COVID-19 arrived," said Patrick J. Cawley, M.D., CEO of MUSC Health. "The MUSC Health Center for Telehealth is to be congratulated for this ability to lead during this crisis."
Since 2012, when MUSC Health adopted EPIC, an electronic health record, the MUSC enterprise has continued to recruit bioinformatics researchers, mainly housed in the Biomedical Informatics Center (BMIC) and Information Solutions, to customize EPIC to the health system's needs and to learn how to improve care by analyzing EHR data.
Existing telehealth tools would prove invaluable to the initiative, but they had to be radically reimagined and integrated for the purpose of responding to COVID-19. Realizing that the scale of the effort would require easy-to-use options, telehealth leaders also onboarded some new tools, such as the user-friendly telemedicine platform doxy.me, created by BMIC researcher Brandon Welch, Ph.D.
"We had a battlefield-type mentality that we had to all get together to form a new structure," said James McElligott, M.D., executive medical director of the MUSC Health Center for Telehealth.
As they worked to build a unified response and fashion existing tools so as to be COVID-19 relevant, telehealth leaders had the full support of hospital leadership, their colleagues in bioinformatics and the South Carolina Clinical & Translational Research Institute, which provided technical and logistical support.
"No one ever said no, even if that meant working for five months straight and into the late hours of the night and calling up Bioinformatics and saying, 'Make this work like this or change it like this,'" said article co-author Kathryn King, M.D., co-director of the MUSC Telehealth Center of Excellence. "No one ever said no because I think we just knew that it had to happen."
MUSC Health chief research information officer and BMIC director Leslie Lenert, M.D., who is senior author of the article, is proud of his bioinformatics team, which put research aside for a time to help meet this urgent clinical need.
"We took the research capacity we had for EPIC support and improvement, and we told them to stop, and we put them on this full time. That's why we were able to respond so fast," said Lenert. "So we took our best people, and we put them on this problem immediately. We protected their time, and we told them to get something done. We started early, we committed absolutely and we worked with our clinicians to solve practical problems that they had."
With BMIC's help and SCTR's support, existing tools were quickly revamped to ensure continuity of care for patients with suspected or confirmed COVID-19 and continued ambulatory care for all other patients.
Virtual urgent care
Virtual urgent care technology, meant to provide patients a convenient way to be seen for minor illnesses, had to be adapted into a platform for screening patients with suspected COVID-19 and scheduling appointments for them at mobile testing sites throughout the state. Previously, patients reporting serious symptoms, such as shortness of breath, would have been kicked out of that system; therefore, Edward O'Bryan, M.D., telemedicine director for the Emergency Department and direct-to-consumer and institutional telehealth at MUSC, along with other telehealth leaders, had to work rapidly with the virtual urgent care vendor to adapt the technology to screen for COVID-19 symptoms. At the same time, they had to begin staffing up to meet the anticipated demand, increasing the number of providers dedicated to virtual urgent care from fewer than ten to more than a hundred. O'Bryan estimates that more than 150,000 patients have now been screened for COVID-19 through the modified virtual urgent care program.
"We were the first people in South Carolina to offer free virtual care COVID screenings," said O'Bryan. "I'm really proud that we were able to roll it out so quickly and that so many South Carolinians took advantage of it."
BMIC researchers developed an artificial intelligence algorithm that could analyze symptom data provided by patients during virtual urgent care screenings and prioritize those most likely to have COVID-19 for testing. The algorithm proved critical when testing capacity was challenged and should continue to play a key role with the implementation nationwide of "batch testing." Essentially, samples from patients thought to be at low risk of having COVID-19 could be tested in batches of five to extend testing capacity. If the test comes back negative, all five patients are presumed to have a negative result. The algorithm helps identify low-risk patients appropriate for such batch testing while reserving individual testing for higher-risk patients.
"What we were able to do is make a very functional system, which, on the outside, might seem simple -you fill out a questionnaire on a telehealth platform, it goes in and everything happens behind the scenes," said McElligott. "But all of that had to be protected for the patient and linked in with the medical record and the lab. We had to know what to do to get testing sites set up with tents and then use the platforms to guide people there. There's just a whole lot of stuff that had to happen to be able to do this: not one patient at a time, but thousands at a time. We couldn't have done it without the Bioinformatics group stepping in and helping to connect all the dots and then bringing new ideas to the table about how to monitor patients."
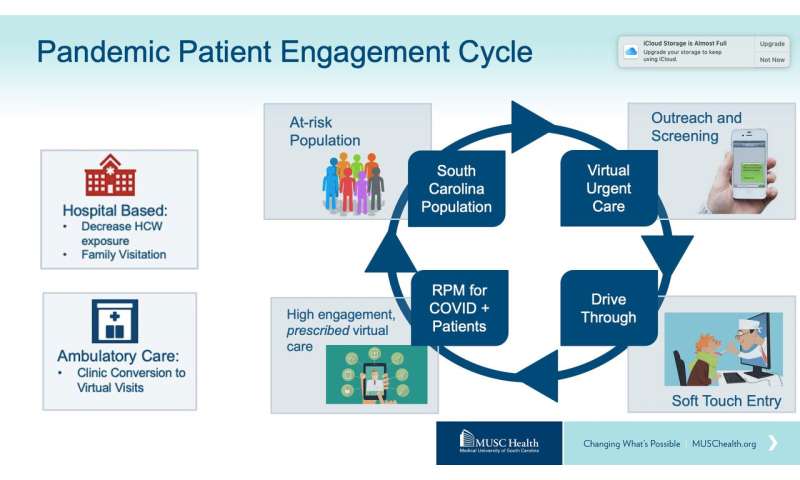
Remote patient monitoring
In the second prong of the four-pronged approach, patients who tested positive were then invited to enroll in a remote patient monitoring (RPM) program. That program, which had been used to track data on patients with chronic disease, was transformed into a virtual means of monitoring and delivering acute care to patients with less severe COVID-19 who were recovering at home. RPM nurses contacted patients by telephone or text to ask if they wished to enroll in the program. Enrolled patients were asked to answer online survey questions daily about the symptoms they were experiencing and to provide temperature and oxygen saturation values. BMIC researchers created a "best practice alert," which notified a patient's RPM nurse should his or her condition begin to deteriorate. The nurse could then call the patient, alert the patient's primary care provider or arrange for a video consultation with a physician at MUSC Health. Patients who developed more severe disease could be hospitalized.
By the end of August, 735 patients had been treated through the RPM program. Of those patients, 20% were considered high risk and 32% medium risk. Some of these patients lived alone or in rural areas, and the daily contact and calls with RPM nurses were an emotional, as well as a medical, lifeline.
"The lead nurse ends up being a connection to care for a pretty decent number of people who are otherwise fairly isolated," said Ford. "They may live in rural areas. They may be elderly and live alone. They're also supposed to be in quarantine, so they're not supposed to be out and about and have people around them. So, it ends up being an important kind of emotional support tool for folks with cases of COVID-19 that are on home quarantine."
Telesitter program
The third prong of the approach, a telesitter program, is intended for patients hospitalized with more severe disease. An audiovisual cart, previously used to monitor patients to keep them from falling, was adapted so that caregivers could monitor and interact with patients with COVID-19 without having to don and doff personal protective gear each time, at the same time limiting the exposure of the health care worker.
"That's been a real satisfier for the clinical teams. They are able to have that kind of ease of communication without having to go into the patient's room each time," said Ford.
Reimagining outpatient care
In addition to ensuring a smooth continuum of care for patients with COVID-19, the team of telehealth and bioinformatics experts also wanted to provide a way for providers to continue to treat all of their patients, not just those with COVID-19. During the lockdown, most in-person outpatient visits were canceled, leaving many patients without needed medical care. Leaders at the Center for Telehealth quickly began preparing to transition most outpatient visits to telehealth visits -a gargantuan task.
"The scale of response was ... it was something I never thought I'd see," said McElligott.
Article co-author Jillian Harvey, Ph.D., associate professor in the Department of Healthcare Leadership and Management at MUSC, agrees.
"Telehealth has always been seen as the promising solution for access to the health care system, but its utilization hasn't picked up as quickly as we expected," explained Harvey. "Now, because of COVID, there has been a huge ramping up of telehealth across the country, especially in March, April and May."
During that timeframe, telehealth visits soared from less than 5% to more than 70% of all visits at MUSC Health. Between March and July, almost 30,000 outpatients met with their physicians via secure video teleconferencing. To make that happen so quickly, the Center for Telehealth, which previously had been predominantly focused on providing services externally to patients in remote areas of the state, suddenly had to integrate itself more deeply into clinical practice at MUSC Health.
"We had to replicate the whole design of the health system in a microcosm," said McElligott.
Typically, he explained, the Center for Telehealth would have smoothed out work processes and flows for such an initiative, but due to the public health emergency, there was no time.
"So, we set up an organizational structure to try to get this done, changed video technologies to more user-friendly ones, built a bunch of tip sheets about how to do it, and we just rolled it out and let everybody innovate."
And innovate they did. Physicians in every specialty took those tip sheets and figured out for themselves how to overcome every obstacle so that they could begin seeing patients virtually.
"So, the true heroes in all of this are the front-line providers who took the information and figured out how to do it themselves because they knew they had to or patients weren't going to be seen," said McElligott.
The way forward
Due to the pandemic, many more providers, payers and patients have become aware of what telehealth can offer. How deeply it will remain integrated into health systems will depend, in part, on whether payers continue to reimburse for telehealth visits at a similar rate as for in-person care, as they are now doing during the public health emergency.
"This ambulatory care conversion required an infrastructure rebuild but is probably the initiative with the most lasting impact," said King. "Now that providers and patients know what telehealth can do, I don't think they will ever give it up."
"There's no real going back to a lack of telehealth use," said McElligott. "That has probably been forever changed."
Indeed, McElligott believes that the pandemic has helped to transform how providers and the public view health care.
"Our health care system has always been very focused on a provider-centric view of health care. In other words, you as a patient come to the provider, and that's how we work," explained McElligott. "Just using distance technologies starts to reverse that. This terrible pandemic has forced a reckoning and a realization that, in terms of the long-term goals of improving health, it's really more important to meet the needs of patients where they're at."
No comments:
Post a Comment