International task force determines current Parkinson's disease subtyping may not fit all patients
The clinical presentation and underlying biology of Parkinson's disease (PD) varies significantly, but attempts to cluster cases into a limited number of subtypes have questionable applicability and relevance, reports the international Task Force for PD Subtypes in the Journal of Parkinson's Disease. Their systematic review of studies reporting a subtyping system for the first time concludes that new approaches are needed that acknowledge the individual nature of the disease and are more aligned with personalized medicine.
03 may 2021--In 2018, the International Parkinson's Disease and Movement Disorders Society (MDS) convened the Task Force for PD Subtypes to critically appraise available PD subtyping studies and to provide guidance for the design and conduct of future studies.
"Subtyping of PD attempts to explain the disease mechanisms, its natural history and, more importantly, to inform therapeutic development, which has justified a large number of studies by different groups over the last 30 years. However, the impact of such efforts remains unclear. They have failed to substantially change the understanding of PD or clinical care thus far. Our current review critically appraises the state of the art in PD subtyping," explained lead authors Tiago A. Mestre, MD, Ph.D., Parkinson's Disease and Movement Disorders Center, Division of Neurology, Department of Medicine, The Ottawa Hospital Research Institute, and Connie Marras, MD, Ph.D., Edmond J. Safra Program in Parkinson's Disease and the Morton and Gloria Shulman Movement Disorders Clinic, Toronto Western Hospital, University Health Network.
The Task Force conducted a systematic review of PD subtypes presented in 38 studies divided into two publication periods (1980-2014 and 2015-2019), which yielded a balanced distribution of included studies into a more recent group representing the current state of the field and older studies to test for temporal trends. They also compared two subtyping methodologic approaches (data-driven versus hypothesis-driven) and critically assessed the methodologic quality and clinical applicability of each study.
The clinical and biological signature of PD may be unique to the individual, rendering PD resistant to meaningful cluster solutions. This review revealed that subtyping studies undertaken to date have significant methodologic shortcomings, and most had questionable clinical applicability and unknown biological relevance. Twenty-six of the studies were cross-sectional and used a data-driven approach. Nonclinical biomarkers were rarely used. Motor characteristics were most commonly reported to differentiate PD subtypes. Most of the studies did not achieve high ratings across a Methodologic Quality Checklist. In a Clinical Applicability Checklist, the clinical importance of differences between subtypes, potential treatment implications, and applicability to the general population were rated poorly, and subtype stability over time and prognostic value were largely unknown.
Quality ratings revealed clear areas for improvement. More extensive use of longitudinal data was regarded as critical for gaining a better understanding of the stability of proposed subtypes and their prognostic value. Although historically, there is a paucity of longitudinal studies, the Task Force found that the use of longitudinal data to define or evaluate subtypes was more common in the last five years due to the public availability of large datasets. They noted that only one study had used longitudinal profiling as the basis for defining subtypes, incorporating data on the evolution of clinical or biological features across time into the definition of subtypes.
The Task Force proposed that serial cluster analyses could provide data about the stability of proposed subtypes and the influence of disease duration on their characteristics. Such approaches could provide additional prognostic value, using information about the early evolution of disease to inform later prognosis or underlying biology.
Contemporary medicine is increasingly focusing on personalized treatment, which extends to patients with PD, noted the Task Force. Subtyping places individuals in groups with similar but not identical features. While this may represent an important step toward identifying individuals who can respond preferentially to certain treatments, placing individuals within a group will inevitably fall short of the truly "personal" goal.
Many of the recommendations in this review could apply to future studies in which the unit of measure is the individual's disease fingerprint rather than the group phenotype, acknowledged the Task Force, while recognizing that such an individual approach poses financial and logistical challenges which will have to be overcome when it comes to clinical trials.
"Having reviewed the existing literature on subtyping and explored the methodologic pitfalls and challenges associated with performing the optimal subtyping studies described above, it is time to reevaluate our approach to understanding and describing PD heterogeneity," commented Dr. Mestre and Dr. Marras. "We have provided recommendations and formulated questions that, once addressed, will inform new approaches to better explain the variability in PD including emphasis on the variability at an individual level, more aligned with future application of personalized medicine principles."
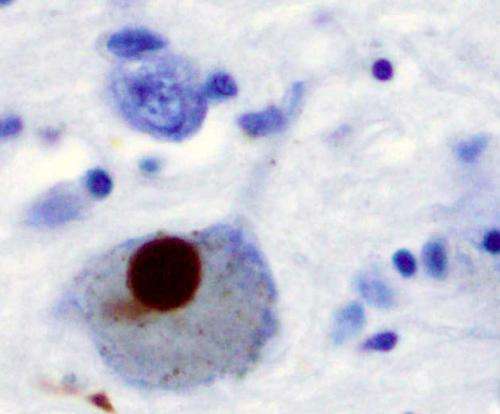
PD is a slowly progressive disorder that affects movement, muscle control, and balance and is characterized by a broad range of motor and non-motor symptoms. It is the second most common age-related neurodegenerative disorder affecting about 3% of the population by the age of 65 and up to 5% of individuals over 85 years of age.
No comments:
Post a Comment