Low-cost ventilatory support for COVID-19 patients
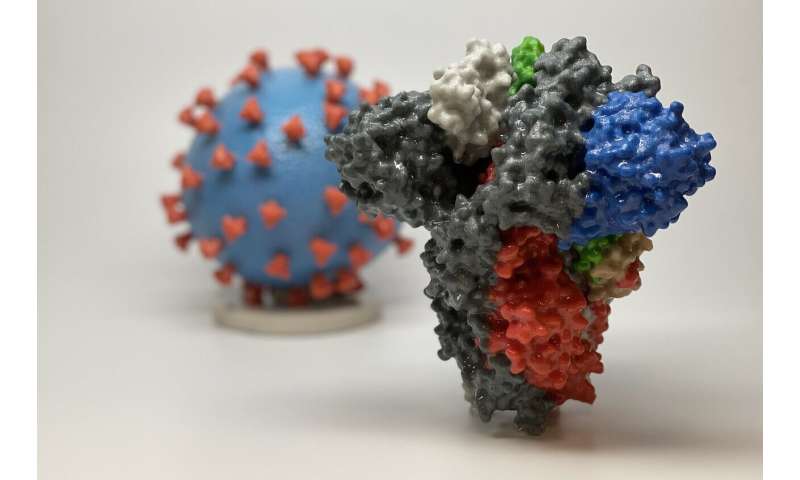
A research team at Leeds has developed a way of creating a ventilatory system for COVID-19 patients that can be made rapidly on a 3-D printer.
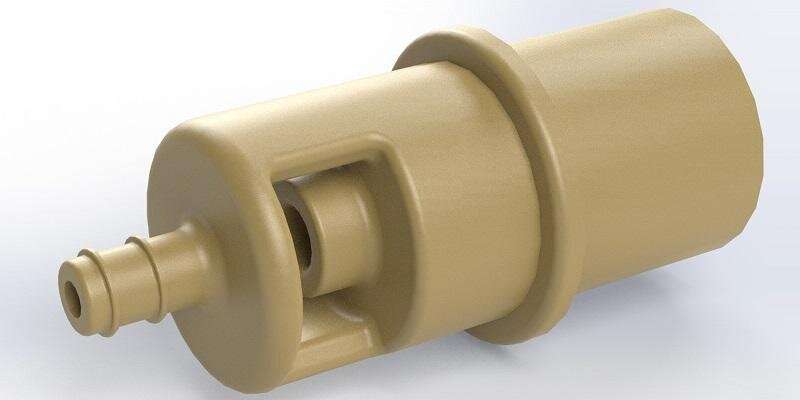
26 april 2020--It is a low-tech solution based on redesigning an existing medical device known as a Venturi valve. It does not need electricity and has no moving parts and could be made in countries without access to advanced manufacturing facilities.
Known as the Leeds Venturi valve, the remodelled device is subject to regulatory approval.
This is the second time in a month that the research team has found a way of repurposing existing medical technology to increase the number of breathing aids available for patients.
In this latest development, the researchers from the University of Leeds, Leeds Teaching Hospitals NHS Trust (LTHT) and Bradford Teaching Hospitals NHS Foundation Trust, focused on the Venturi valve—a small plastic device normally used to increase the flow of oxygen to a patient.
One end of the valve is attached to the oxygen-supply pipe by a patient's bed or to an oxygen cylinder. The other end connects to the tubing that goes to the person's oxygen mask.
The repurposed device not only delivers an increased flow of oxygen to the patient, it also raises the pressure of that flow, opening the tiny air sacs in the lungs that are damaged by the virus and allowing oxygen to get into the body.
Importantly, the device produces an effect similar to a continuous positive airway pressure, or CPAP, machine—a form of intermediate-level ventilator capable of delivering oxygen at the right concentration and pressure to have a therapeutic effect.
Medical reports from China have indicated that moderately ill people can be treated on CPAP machines and avoid the need for full mechanical ventilation, which is often only available in hospital intensive care units and required for the sickest patients.
Dr. Tom Lawton, Consultant in Critical Care and Anaesthesia at Bradford Teaching Hospitals, who collaborated on the project, said: "We are already seeing that treating COVID-19 patients with CPAP can help avoid the need for ventilators and intensive care; the key is to do this in a resource-efficient way.

"Devices like this venturi valve could be a key to expanding the use of CPAP across the globe."
Maxillofacial Surgeon Jiten Parmar, from Leeds Teaching Hospitals NHS Trust, another member of the research team, said: "This collaborative work has allowed for the innovation of a therapeutic oxygen delivery device for use in countries where there may be a lack of CPAP machines or oxygen supply."
Two weeks ago, the researchers announced details of how a device used to help people with a condition called sleep apnoea could be adapted to treat COVID-19 patients. There are thought to be thousands of machines across the NHS that could be used this way.
Dr. Pete Culmer, Associate Professor in the School of Mechanical Engineering at the University of Leeds, said: "Our work has focused on investigating more rapid ways of getting life-saving technology to the side of patients as the pandemic spreads.
"Across the world, there have been concerns about increasing the number of ventilators that are available. We have now looked at two solutions. Both involve adapting existing technologies and that dramatically reduces the time it takes to get equipment to the patient's bedside.
"Taking established technology and repurposing it means there is a greater chance that we can make real our solutions in a timely and effective way."
The researchers have put their findings online.
Nikil Kapur, Professor of Applied Fluid Mechanics in the School of Mechanical Engineering, leads the research team. He said: "We set out to make sure that the Leeds Venturi valve had two significant improvements over existing Venturi valves.
"One, that they made efficient use of hospital oxygen supplies—vital given that the demand on supplies is likely to be high—and two, that they could be easily manufactured.
"As the pandemic sweeps across the world, researchers need to think about solutions and technologies that can be implemented in developing countries. This is one of those solutions."
Venturi valves are not new devices and are based on observations made by Italian physicist Giovanni Venturi in the late 1700s.
More information: Peter Culmer et al. Delivery of CPAP respiratory support for COVID-19 using repurposed technologies, (2020). DOI: 10.1101/2020.04.06.20055665
Provided by University of Leeds