The development of 5G significantly increased the health of older adults, study finds
The Chinese government attaches great importance to the construction of Fifth Generation Mobile Communication Technology infrastructure (5G), which has been shown in a new study to play a positive role in the self-rated health of older adults in mainland China, indicating the health-promoting effects of technological advances.
14 oct 2023--China has built one of the largest and most technologically advanced 5G networks, and 5G industry applications have been integrated into more than 60 national economic categories including the medical and health care industries, aiming at meeting the growing medical and health needs of the people. However, as a new and emerging technology, the impact of 5G on public health at the national level has not been well elucidated with reliable empirical evidence.
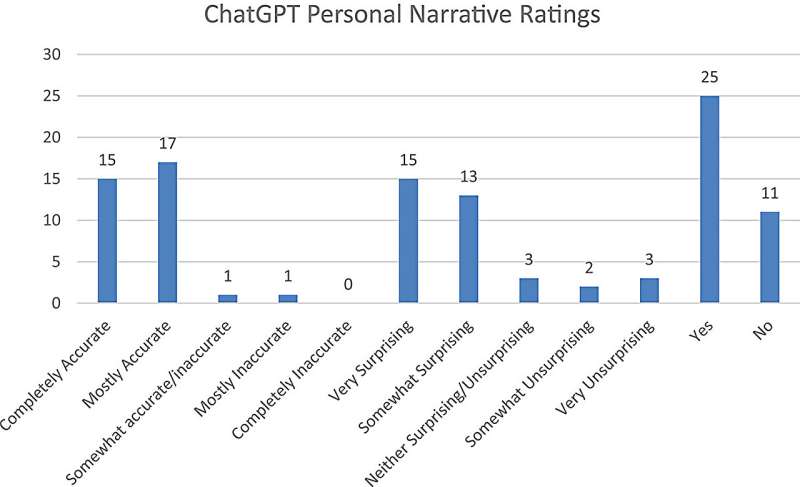
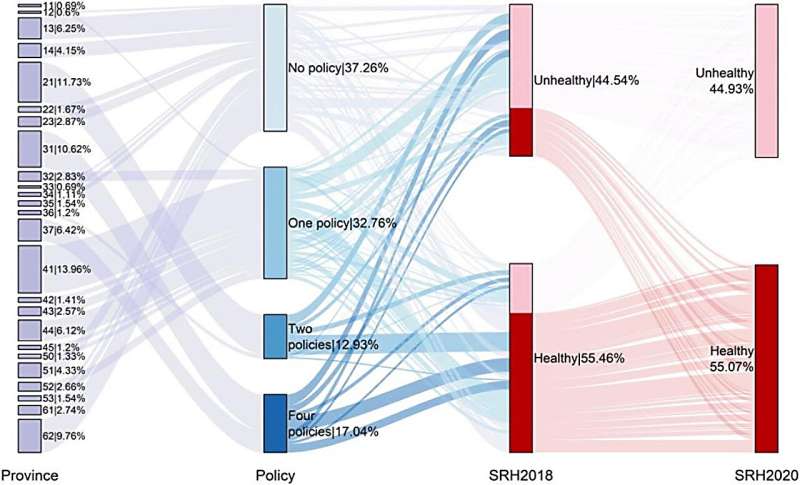
In our study published in Global Transitions, we explored the effects of 5G development on self-rated health (SRH) among older adults with different sociodemographic features in mainland China. Using the nationally representative data from the China Family Panel Studies (CFPS) in 2018 and its follow-up in 2020, we used the development of 5G as a natural experiment to capture the impact of 5G development on the health of older adults.
Older adults from provinces with 5G policies in varying levels between 2018 and 2020 were considered as the exposure group while others were considered as the reference group, and the differences in SRH of the older adults were compared in provinces with different numbers of policies.
The health effects of 5G development
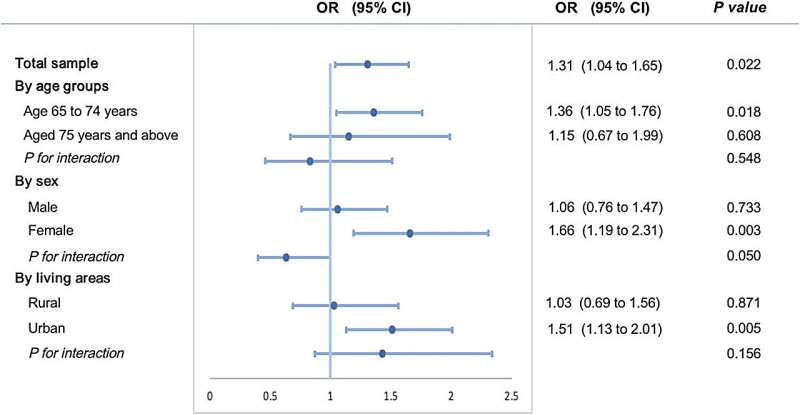
Our findings revealed that the development of 5G significantly increased the SRH of older adults. After the enactment of the 5G policies, the probability of self-rated good health increased by 31% for each unit increase in the development level of 5G policies. And there were notable disparities in age group, gender and living areas.
The improvement effect of the 5G policies on SRH was intensified in the younger cohort, those aged 65 to 74 years, females, and those living in urban areas. The probability of self-rating good health of older adults aged 75 years and above, males, and those living in rural areas also increased after being exposed to the 5G policies but was not statistically significant.
Public health facilitated by technological development
To the best of our knowledge, our study provides novel insights into the impact of 5G development on the SRH of older adults for the first time. The findings are that 5G development has a positive effect on the SRH of older adults and SRH is found to be particularly improved in the 65- to 74-year-old groups, female groups, and urban participants.
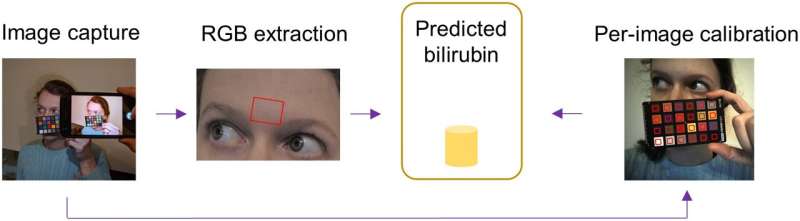
The introduction of 5G policy provides a micro-opportunities and a macro-environment for older adults to promote their health status. At the micro level, 5G enables more older adults to use smart devices and access the internet, facilitating access to health information and promoting social participation. At the macro level, 5G-related application in the medical and health care industry contributes to meeting the medical and health needs of the older adults.
However, considering the heterogeneity, some older adults are in the economic, health and digital divide at the same time, and the gap between them and the older adults who occupy the advantage of digital resources is gradually increasing with the trend of technology development. Target measures should be adopted to avoid worsening inequality and improve the health of all older adults.
We hope that the fast penetration of digital technologies such as 5G will facilitate and scale up the innovations that can create and spread health, allowing public health to fulfill it vision of everyone, regardless of gender and age, being able to enjoy a healthy life at last.
More information: Huameng Tang et al, The effect of 5G policy development on self-rated health among Chinese older adults: A quasi-experimental study, Global Transitions (2023). DOI: 10.1016/j.glt.2023.08.002