Obstructive sleep apnea may directly cause early cognitive decline

Obstructive sleep apnea (OSA) is a potentially dangerous condition. During sleep, the throat muscles of people with OSA relax and block the airflow into the lungs, so that they repeatedly stop breathing. Common symptoms of OSA include restless sleep, loud snoring, daytime sleepiness, and prolonged headaches in the morning—highly debilitating for patients and their partners.
09 april 2023--OSA is currently underdiagnosed: it may occur in as much as 15 to 30% of men and 10 to 15% of women, or approximately 1 billion adults worldwide, of whom an estimated 80% don't know they have it. Major risk factors for OSA include middle or old age, being obese, smoking, chronic nasal blockage, high blood pressure, and being male.
Now, researchers from the UK, Germany, and Australia have shown for the first time that in middle-aged men, OSA can also cause early cognitive decline, even in patients who are otherwise healthy and not obese. The results are published in Frontiers in Sleep.
"We show poorer executive functioning and visuospatial memory and deficits in vigilance, sustained attention, and psychomotor and impulse control in men with OSA. Most of these deficits had previously been ascribed to co-morbidities," said Dr. Ivana Rosenzweig, a neuropsychiatrist who heads the Sleep and Brain Plasticity Centre at King's College London, and the lead author of the study.
"We also demonstrated for the first time that OSA can cause significant deficits in social cognition."
Rare cohort without co-morbidities
Rosenzweig and colleagues studied a group of 27 men between the ages of 35 and 70 with a new diagnosis of mild to severe OSA but without any co-morbidities. Such patients are relatively rare, because most men and women with OSA have co-morbidities such as cardiovascular and metabolic disease, stroke, diabetes, chronic systemic inflammation, or depression.
The men were not currently smokers or alcohol abusers, and were not obese (i.e., with a body mass index (BMI) below 30). As a control, the researchers studied a group of seven age-, BMI-, and education-matched men without OSA. The OSA diagnosis was confirmed by a so-called WatchPAT test of their respiratory function during sleep at home, and also by video-polysomnography at King's College sleep center.
With the latter method, the brain waves of sleeping subjects were measured by electroencephalography (EEG), while their blood oxygen levels, heart rate, breathing, and eye and leg movements were tracked.
The scientists also tested the subjects' cognitive function with the CANTAB or 'Cambridge Neuropsychological Test Automated Battery' of tests.
Premature cognitive decline
The results showed that patients with severe OSA had poorer vigilance, executive functioning, short-term visual recognition memory, and social and emotion recognition than the matched controls. Patients with mild OSA performed better in these domains than patients with severe OSA, but worse than the controls.
"The most significant deficits…were demonstrated in the tests that assess both simultaneous visual matching ability and short-term visual recognition memory for non-verbalizable patterns, tests of executive functioning and cued attentional set shifting, in vigilance and psychomotor functioning, and lastly, in social cognition and emotion recognition," wrote the authors.
The authors conclude that OSA is sufficient to cause these cognitive deficits, which previous studies had attributed to the most common co-morbidities of OSA such as systemic hypertension, cardiovascular and metabolic diseases, and type 2 diabetes.
Unclear mechanism
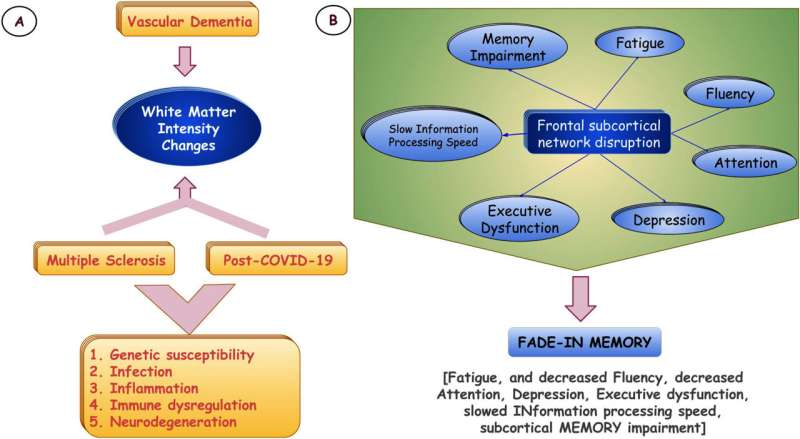
But what is the mechanism by which OSA causes premature cognitive decline? The authors speculated that the cognitive deficits are due to intermittent low oxygen and high carbon dioxide in the blood, changes in blood flow to the brain, sleep fragmentation, and neuroinflammation in OSA patients.
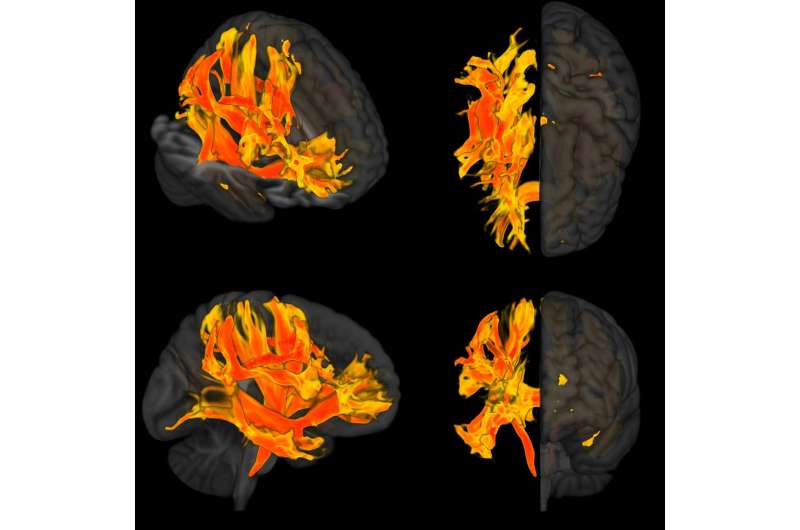
"This complex interplay is still poorly understood, but it's likely that these lead to widespread neuroanatomical and structural changes in the brain and associated functional cognitive and emotional deficits," said Rosenzweig.
Whether co-morbidities have similar negative effects on cognition above and beyond those caused directly by OSA is not yet clear.
"Our study is a proof of concept. However, our findings suggest that co-morbidities likely worsen and perpetuate any cognitive deficits caused directly by OSA itself," said Rosenzweig.
"What remains to be clarified in future studies is whether co-morbidities have an additive or synergistic effect on the latter deficits, and whether there is a difference in brain circuitry in OSA patients with or without co-morbidities."
More information: Ivana Rosenzweig et al, Distinct cognitive changes in male patients with obstructive sleep apnea without co-morbidities, Frontiers in Sleep (2023). DOI: 10.3389/frsle.2023.1097946 , www.frontiersin.org/articles/1 … le.2023.1097946/full