Calorie restriction slows pace of aging in healthy adults

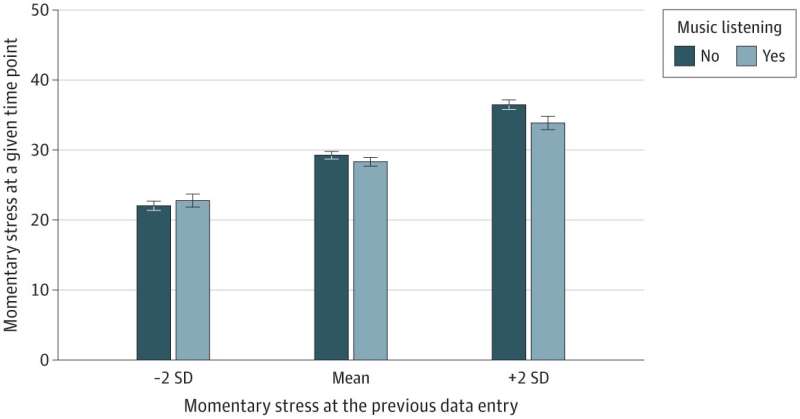
In a first of its kind randomized controlled trial an international team of researchers led by the Butler Columbia Aging Center at the Columbia University Mailman School of Public Health shows that caloric restriction can slow the pace of aging in healthy adults. The CALERIE intervention slowed pace of aging measured from participants' blood DNA methylation using the algorithm DunedinPACE (Pace of Aging, Computed from the Epigenome). The intervention effect on DunedinPACE represented a 2-3 percent slowing in the pace of aging, which in other studies translates to a 10-15 percent reduction in mortality risk, an effect similar to a smoking cessation intervention. The results are published online in the journal Nature Aging.
26 fev "In worms, flies, and mice, calorie restriction can slow biological processes of aging and extend healthy lifespan" says senior author Daniel Belsky, Ph.D., associate professor of epidemiology at Columbia Mailman School and a scientist with Columbia's Butler Aging Center. "Our study aimed to test if calorie restriction also slows biological aging in humans."
The CALERIE Phase-2 randomized controlled trial is the first ever investigation of the effects of long-term calorie restriction in healthy, non-obese humans. The trial randomized 220 healthy men and women at three sites in the U. S. to a 25 percent calorie-restriction or normal diet for two years. CALERIE is an acronym for 'Comprehensive Assessment of Long-Term Effects of Reducing Intake of Energy'.
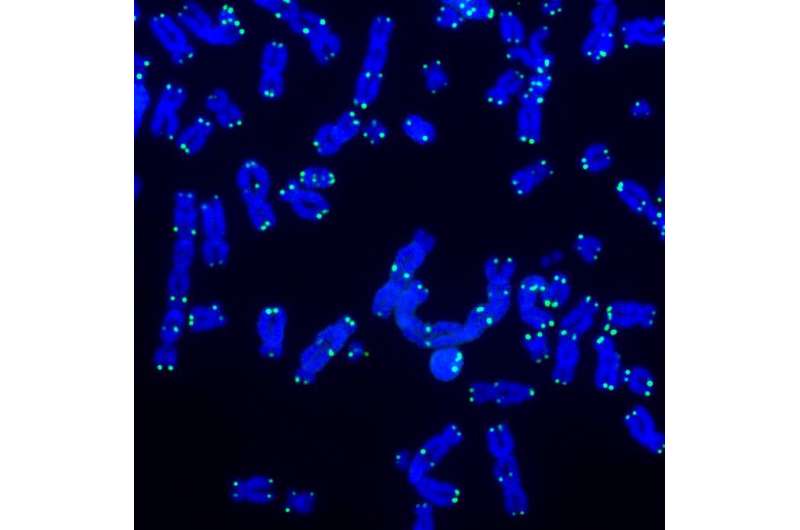
To measure biological aging in CALERIE Trial participants, Belsky's team analyzed blood samples collected from trial participants at pre-intervention baseline and after 12- and 24-months of follow-up. "Humans live a long time," explained Belsky, "so it isn't practical to follow them until we see differences in aging-related disease or survival. Instead, we rely on biomarkers developed to measure the pace and progress of biological aging over the duration of the study." The team analyzed methylation marks on DNA extracted from white blood cells. DNA methylation marks are chemical tags on the DNA sequence that regulate the expression of genes and are known to change with aging.
In the primary analysis Belsky and colleagues focused on three measurements of the DNA methylation data, sometimes known as "epigenetic clocks". The first two, the PhenoAge and GrimAge clocks, estimate biological age, or the chronological age at which a person's biology would appear "normal". These measures can be thought of as "odometers" that provide a static measure of how much aging a person has experienced. The third measure studied by the researchers was DunedinPACE, which estimates the pace of aging, or the rate of biological deterioration over time. DunedinPACE can be thought of as a "speedometer".
"In contrast to the results for DunedinPace, there were no effects of intervention on other epigenetic clocks," noted Calen Ryan, Ph.D., Research Scientist at Columbia's Butler Aging Center and co-lead author of the study. "The difference in results suggests that dynamic 'pace of aging' measures like DunedinPACE may be more sensitive to the effects of intervention than measures of static biological age."
Our study found evidence that calorie restriction slowed the pace of aging in humans" Ryan said. "But calorie restriction is probably not for everyone. Our findings are important because they provide evidence from a randomized trial that slowing human aging may be possible. They also give us a sense of the kinds of effects we might look for in trials of interventions that could appeal to more people, like intermittent fasting or time-restricted eating."
A follow-up of trial participants is now ongoing to determine if the intervention had long-term effects on healthy aging. In other studies, slower DunedinPACE is associated with reduced risk for heart disease, stroke, disability, and dementia. "Our study of the legacy effects of the CALERIE intervention will test if the short-term effects observed during the trial translated into longer-term reduction in aging-related chronic diseases or their risk factors," says Sai Krupa Das, a senior scientist and CALERIE investigator who is leading the long-term follow up of CALERIE participants.
DunedinPACE was developed by Daniel Belsky and colleagues at Duke University and the University of Otago. To develop DunedinPACE, researchers analyzed data from the Dunedin Longitudinal Study, a landmark birth cohort study of human development and aging that follows 1000 individuals born in 1972-73 in Dunedin, New Zealand. Researchers first analyzed the rate of change in 19 biomarkers across 20 years of follow-up to derive a single composite measure of the Pace of Aging. Next, the researchers used machine-learning techniques to distill this 20-year Pace of Aging into a single-time-point DNA methylation blood test. The values of the DunedinPACE algorithm correspond to the years of biological aging experienced during a single calendar year, providing a measure of the pace of aging.
More information: Daniel Belsky, Effect of long-term caloric restriction on DNA methylation measures of biological aging in healthy adults from the CALERIE trial, Nature Aging (2023). DOI: 10.1038/s43587-022-00357-y. www.nature.com/articles/s43587-022-00357-y