Older Australians need to consider home modifications sooner
Most older Australians would prefer to remain in their home for as long as possible, but few consider age-friendly modifications that reduce safety risks and ensure they avoid injuries during their golden years, according to new research.
08 Jun 2023--Flinders University researchers interviewed 16 Adelaide residents aged between 52 and 76 about their own or their relatives future housing plans and current living arrangements.
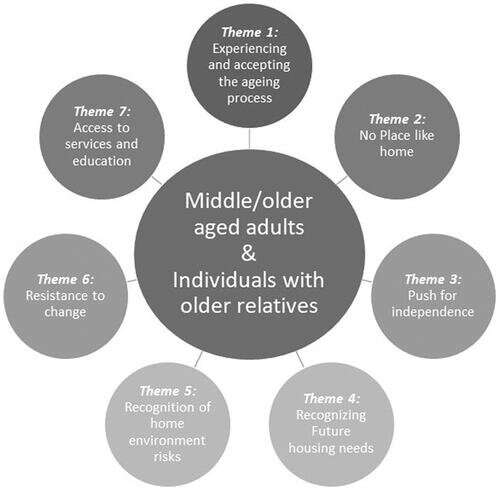
The journal article, "Considering the home environment and planning for the future: A qualitative exploration of the views of older adults and individuals with older relatives," published in the Scandinavian Journal of Occupational Therapy, determined that older people planning to age gracefully at home lack the information they need to properly assess safety risks so they can undertake renovations to address them.
Although older people and their family members reported some knowledge about home modifications that could be made, most participants agreed that more information and tools to help with future planning would be beneficial.
The new research by Roslyn Dalistan, Associate Professor Kate Laver and Professor Stacey George highlights key challenges for older people seeking to age in place after the federal government established a new taskforce to review the new in-home care program in the federal budget, which will commence in 2025. The study reveals that many older Australians are living in homes with clear dangers, hazards, and limited accessibility as they age, but few are addressing these challenges properly.
Most common potential hazards and solutions:
High maintenance garden (without irrigation system)
- Consider reducing garden maintenance needs (plants that don't need much water or pruning, low maintenance landscaping, irrigation systems)
All entrances to the house have one or more steps
- Consider how one entry could be modified for easy access if a wheelchair or wheeled walking frame was required in future (e.g., ramp)
Step or ledge present between shower cubicle and bathroom floor
- Consider bathroom alterations to ensure smooth transition between cubicle and floor
Slippery bathroom tiles
- Consider application of non-slip treatment
- If renovating, choose tiles which are not slippery when wet
Toilet door swings inward
- Have the swing of the door changed so that it swings outwards.
Chairs in living room are low and/or soft
- When purchasing new chairs, purchase chairs that are firm, supportive and not too low (height depends on height of individual). Armrests can be helpful.
The researchers have designed and tested a digital tool with 60 older people to assist with identifying and eliminating risks and are planning to make it freely available to the public in the near future.
Registered occupational therapist at Flinders University, Associate Professor Kate Laver, says older people prefer to stay at home for several reasons, including a sense of attachment to the home, the high costs of moving in today's real estate market, and a desire to maintain existing social and community networks.
"Home is considered by older adults to be a place of comfort and safety where independence can be preserved. Strong community networks enable older adults to cope with age-related changes and prevent isolation. Being surrounded by important possessions or memories is also linked to their quality of life," says Professor Laver.
"However, our ability to function independently within the home environment can become increasingly difficult. Most participants in our study accepted the aging process and could recognize hazards and potential risks. However, others were determined to remain independent at home and resistant to making future changes until necessary."
"They were all interested in obtaining more information about how to improve home safety or services to support aging in place. This shows we need tools that enable older people and their families to properly self-assess their own homes. This tool will be available both in hard copy and as a digital tool and will be used to promote and support future planning."
Study co-author and Flinders University Professor Stacey George says the research shows that decision-making around home safety among the aging population can be compromised by a lack of awareness, inadequate access to information, and the sudden onset of age-related changes.
"It's why an education guide or tool to support forwards planning and housing decisions may improve early awareness among Australia's aging population."
More information: Roslyn Dalistan et al, Considering the home environment and planning for the future: A qualitative exploration of the views of older adults and individuals with older relatives, Scandinavian Journal of Occupational Therapy (2023). DOI: 10.1080/11038128.2023.2192027