Study suggests strong sense of purpose in life promotes cognitive resilience among middle-aged adults
New research suggests that having a stronger purpose in life (PiL) may promote cognitive resilience among middle-aged adults. Cognitive resilience refers to the capacity of the brain to cope with stressors, injuries and pathology, and resist the development of symptoms or disabilities. Furthermore, having a purposeful life implies changes in the organization of the brain with one specific brain network, the dorsal Default Mode Network, showing greater functional connections within its components and with other brain areas. This may represent a neuroprotection mechanism that ultimately ensures better cognitive function into old age.
10 may 2023--These are among the findings in the article, "Purpose In Life Promotes Resilience To Age-Related Brain Burden And Neuroprotection Through Functional Connectivity In Middle-Aged Adults," published in the journal Alzheimer's Research & Therapy.
"The present data extend previous findings found in advanced age and pathological aging, such as Alzheimer's Disease, revealing that having a strong sense of purpose might confer resilience already in middle age," said author Dr. Kilian Abellaneda-Pérez, Departament de Medicina, Facultat de Medicina i Ciències de la Salut, Institut de Neurociències, Universitat de Barcelona, Barcelona, Spain.
"The fact that individuals in the higher purpose in life group had greater connectivity between specific Dorsal default-mode network nodes, which correlated with cognitive performance, suggest such changes in the functional organization of the brain may represent the mechanism by which a greater purpose in life promotes brain health and protects the brain from dysfunction even in the face of stress, adversity and illness," said Dr. Alvaro Pascual-Leone, Medical Director, Deanna and Sidney Wolk Center for Memory Health at Hebrew SeniorLife; and Department of Neurology, Harvard Medical School.
He concludes, "What is also exciting is that each of us, with appropriate guidance and support, can develop and sustain a robust sense of purpose and thus contribute to our brain health and well-being."
Disease-modifying agents to counteract cognitive impairment in older age remain elusive. Hence, identifying modifiable factors promoting brain reserve and resilience is paramount. In Alzheimer's disease, education and occupation are typical reserve proxies. However, the importance of psychological factors is being increasingly recognized, as their operating biological mechanisms are elucidated.
Purpose in life, one of the pillars of psychological well-being, has previously been found to reduce the deleterious effects of Alzheimer's Disease-related pathological changes on cognition. However, whether purpose in life operates as a cognitive resilience factor in middle-aged individuals, and what are the underlying neural mechanisms remains unknown.
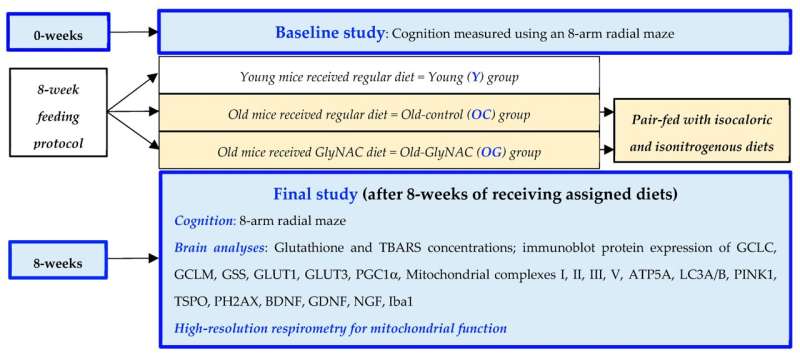
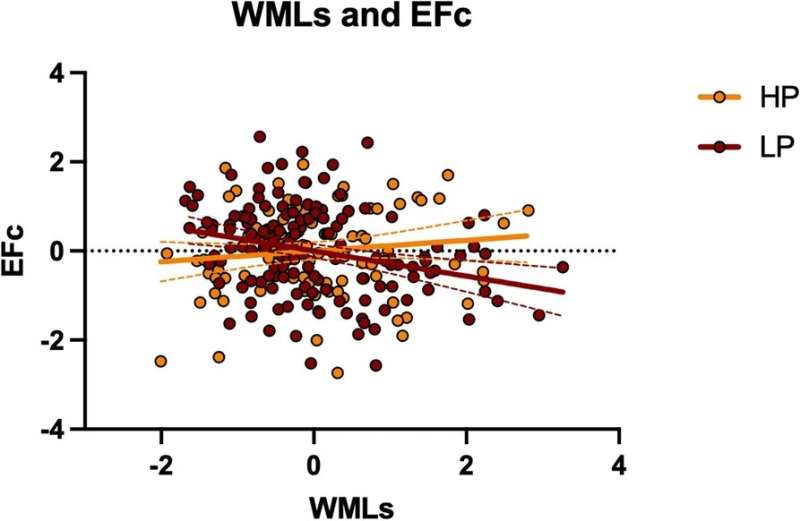
Data was obtained from 624 middle-aged adults (mean age 53.71±6.9; 303 women) from the Barcelona Brain Health Initiative cohort. Individuals with lower (N=146) and higher (N=100) purpose in life (PiL) rates, according to the division of this variable into quintiles, were compared in terms of cognitive status, a measure reflecting brain burden (white matter lesions; WMLs), and resting-state functional connectivity (rs-FC), examining system segregation (SyS) parameters using 14 common brain circuits.
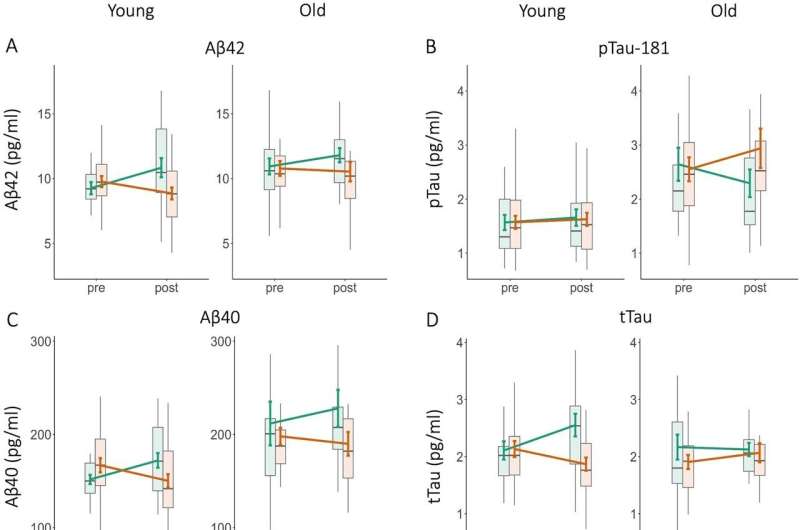
Neuropsychological status and WMLs burden did not differ between PiL groups. However, in the lower PiL group greater WMLs entailed a negative impact on executive functions. Subjects in the higher PiL group showed lower SyS of the dorsal DMN (dDMN), indicating lesser segregation of this network from other brain circuits.
Specifically, higher PiL individuals had greater inter-network connectivity between specific dDMN nodes, including the frontal cortex, the hippocampal formation, the midcingulate region, and the rest of the brain. Greater functional connectivity in some of these nodes positively correlated with cognitive performance.
More information: Kilian Abellaneda-Pérez et al, Purpose in life promotes resilience to age-related brain burden in middle-aged adults, Alzheimer's Research & Therapy (2023). DOI: 10.1186/s13195-023-01198-6