Leprosy drug holds promise as at-home treatment for COVID-19

A Nature study authored by scientists at Sanford Burnham Prebys Medical Discovery Institute and the University of Hong Kong shows that the leprosy drug clofazimine, which is FDA approved and on the World Health Organization's List of Essential Medicines, exhibits potent antiviral activities against SARS-CoV-2 and prevents the exaggerated inflammatory response associated with severe COVID-19. Based on these findings, a Phase 2 study evaluating clofazimine as an at-home treatment for COVID-19 could begin immediately.
20 mar 2021--"Clofazimine is an ideal candidate for a COVID-19 treatment. It is safe, affordable, easy to make, taken as a pill and can be made globally available," says co-senior author Sumit Chanda, Ph.D., professor and director of the Immunity and Pathogenesis Program at Sanford Burnham Prebys. "We hope to test clofazimine in a Phase 2 clinical trial as soon as possible for people who test positive for COVID-19 but are not hospitalized. Since there is currently no outpatient treatment available for these individuals, clofazimine may help reduce the impact of the disease, which is particularly important now as we see new variants of the virus emerge and against which the current vaccines appear less efficacious."
Promising candidate revealed by screening drug library
Clofazimine was initially identified by screening one of the world's largest collections of known drugs for their ability to block the replication of SARS-CoV-2. Chanda's team previously reported in Nature that clofazimine was one of 21 drugs effective in vitro, or in a lab dish, at concentrations that could most likely be safely achieved in patients.
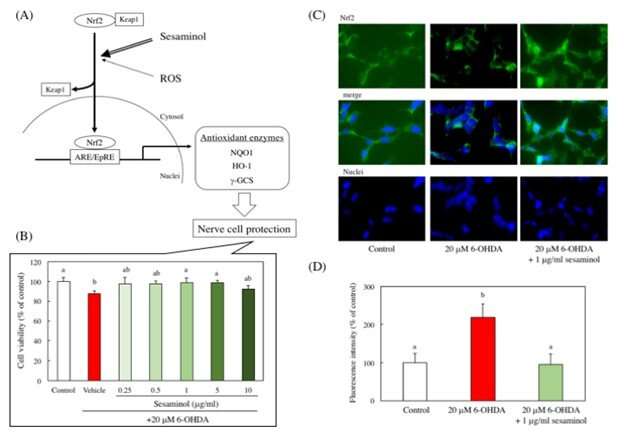
In this study, the researchers tested clofazimine in hamsters—an animal model for COVID-19—that were infected with SARS-CoV-2. The scientists found that clofazimine lowered the amount of virus in the lungs, including when given to healthy animals prior to infection (prophylactically). The drug also reduced lung damage and prevented "cytokine storm," an overwhelming inflammatory response to SARS-CoV-2 that can be deadly.
"The animals that received clofazimine had less lung damage and lower viral load, especially when receiving the drug before infection," says co-senior author Ren Sun, Ph.D., professor at the University of Hong Kong and distinguished professor emeritus at the University of California, Los Angeles (UCLA). "Besides inhibiting the virus, there are indications that the drug also regulates the host response to the virus, which provides better control of the infection and inflammation."
Clofazimine also worked synergistically with remdesivir, the current standard-of-care treatment for people who are hospitalized due to COVID-19, when given to hamsters infected with SARS-CoV-2. These findings suggest a potential opportunity to stretch the availability of remdesivir, which is costly and in limited supply.
How clofazimine works
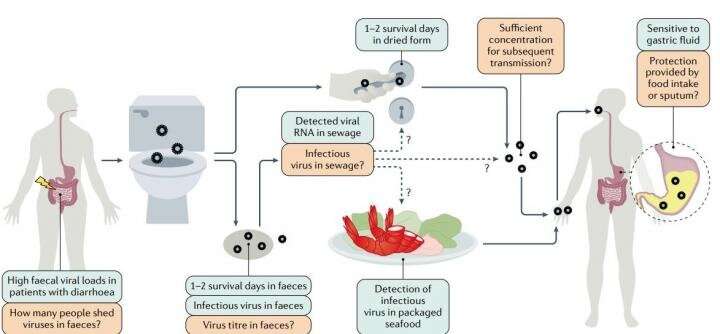
The study showed that clofazimine stops SARS-CoV-2 infection in two ways: blocking its entry into cells and disrupting RNA replication (SARS-CoV-2 uses RNA to replicate). Clofazimine was able to reduce the replication of MERS-CoV, the coronavirus that causes Middle East Respiratory Syndrome (MERS), in human lung tissue.
"Potentially most importantly, clofazimine appears to have pan-coronavirus activity, indicating it could be an important weapon against future pandemics," says co-senior author Kwok-Yung Yuen, M.D., chair of Infectious Diseases at the University of Hong Kong, who discovered the coronavirus that causes severe acute respiratory syndrome (SARS). "Our study suggests that we should consider creating a stockpile of ready-made clofazimine that could be deployed immediately if another novel coronavirus emerges."
In July 2020 Sumit Chanda shared more about his team's race to find a treatment for COVID-19.
Testing clofazimine in the clinic
A Phase 2 trial evaluating clofazimine in combination with interferon beta-1b as a treatment for people with COVID-19 who are hospitalized is ongoing at the University of Hong Kong. Interferon beta-1b is an immunoregulator that is given as an injection and is currently used to treat people with multiple sclerosis.
"Our data suggests that clofazimine should also be tested as a monotherapy for people with COVID-19, which would lower many barriers to treatment," says Chanda. "People with COVID-19 would be able to simply receive a regime of low-cost pills, instead of traveling to a hospital to receive an injection."