Surgical stabilization of odontoid fractures shown to improve outcomes
Odontoid fractures—those occurring in the second cervical vertebra—are common in elderly patients after a low-energy fall. However, whether the initial treatment should be surgical or non-operative still isn't known. Previous studies haven't accounted for differences in injury severity, or the presence or absence of neurologic impairment, which can affect patients' results.
09 Jul 2023--On this topic, an article titled "Surgery Decreases Nonunion, Myelopathy, and Mortality for Patients with Traumatic Odontoid Fractures: A Propensity Score Matched Analysis" is published in the journal Neurosurgery.
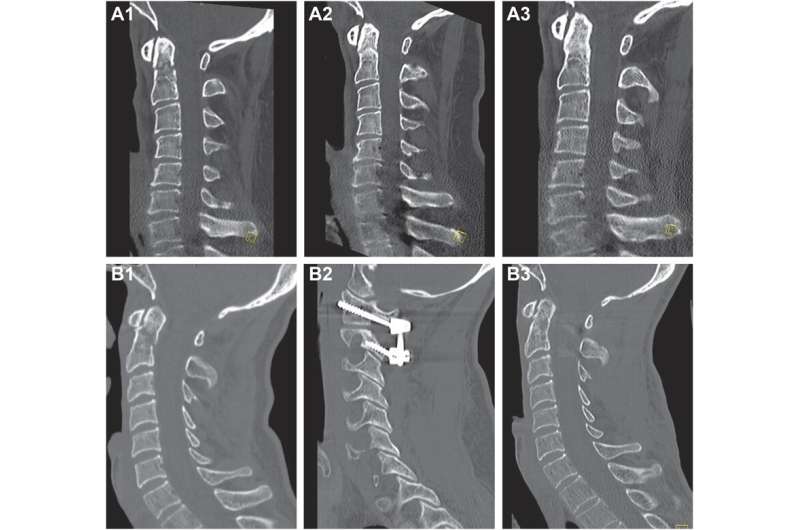
Michael B. Cloney, MD, MPH, of the Department of Neurological Surgery at Northwestern University in Chicago, and colleagues have published evidence that surgery should be considered as the initial approach for many patients. Compared with non-operative approaches to treatment, surgical stabilization of the fracture was associated with less myelopathy (mobility impairment due to spinal cord damage), and lower rates of fracture non-union, 30-day mortality, and one year mortality.
"Given the increasing incidence of odontoid fractures with the aging population, we believe our findings could assist with neurosurgical decision-making for an increasingly common and complex problem," the researchers say.
Propensity score matching: A way to account for nonrandomized patient groups
Dr. Cloney and his colleagues reviewed initial treatment data on 296 patients who were cared for at Northwestern Memorial Hospital between January 1, 2010, and December 31, 2020, because of an odontoid fracture. Their average age was 73. During the hospitalization, 22% had surgery and 78% had non-operative treatment (5% were immobilized in a halo-vest and 73% received a cervical collar).
Since the patients weren't randomized to these treatments, the research team used a type of analysis called propensity score adjustment. They calculated "propensity scores" for each individual—the probability that the patient would have been assigned to receive one of the two treatment approaches based on certain characteristics.
For example, to study the effect of surgery on mortality rates, patients were matched on age, sex, Injury Severity Score, Nurick score (a measure of myelopathy), their number of chronic diseases and chronic conditions such as smoking, and whether they had to be admitted to the intensive care unit.
Surgical stabilization leads to better results
Follow up with patients lasted an average of 45 weeks. On the propensity score-matched analyses, the group that underwent surgery showed significantly better outcomes than the non-operative group:
- Lower rate of fracture non-union—39.7% vs. 57.3%; treatment effect, 15% less risk of nonunion
- Lower 30-day mortality rate—1.7% vs. 13.8%; treatment effect, 10% less risk of death
- Lower one year mortality rate—7.0% vs. 23.7%; treatment effect, 10% less risk of death
Other analyses showed patients in the surgery group were 52% less likely than those in the non-operative group to have poor Nurick scores at the 26-week postoperative follow-up visit and were 41% less likely to die during the overall follow-up period. Both differences were statistically significant.
"The mortality benefit calculated in the existing literature typically represents an unadjusted mortality rate between two potentially different populations, which leaves it liable to confounding," the authors note. "Our study represents a relatively large institutional series that suggests a benefit from surgical stabilization in this population while controlling for confounding factors more thoroughly than existing literature."
More information: Michael Cloney et al, Surgery Decreases Nonunion, Myelopathy, and Mortality for Patients With Traumatic Odontoid Fractures: A Propensity Score Matched Analysis, Neurosurgery (2023). DOI: 10.1227/neu.0000000000002557
No comments:
Post a Comment